
Highmark Blue Shield of Northeastern New York (BSNENY) is aligning with the Centers for Medicare and Medicaid Services (CMS) guidelines, which only accept the use of Current Procedural Terminology (CPT) code 99499 for additional diagnosis codes for risk adjustment. Please use CPT code 99499 instead of 99080 to accurately capture a patient’s active chronic condition(s).
It is important that you document all active chronic conditions and submit the diagnosis codes on a claim at least once per calendar year. The additional codes provide a more accurate picture of the member’s health.
Instructions for SubmittingCPT code 99499 will show as denied/rejected for payment on the Explanation of Benefits (EOB); however, Highmark will still capture the diagnosis codes affiliated with this procedure code.
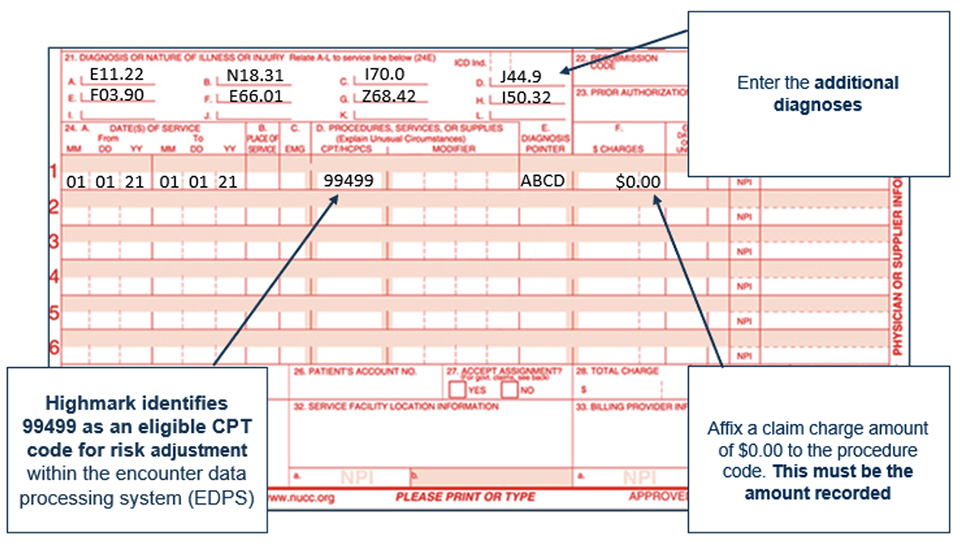
Details on risk adjustment programs and submitting claims with additional diagnosis codes are included in Chapter 5, Unit 6 (Quality Management) of the Highmark Provider Manual  which can be found on the Provider Resource Center.
which can be found on the Provider Resource Center.